Basic guide for using CDC data to understand how many people must die for a society to reach herd immunity (also posted on Medium)

An epidemic is not a single number. Knowing exactly how bad an epidemic is requires knowing both how quickly it is going to spread and how bad its effects will be on those who are affected by it. To make matters worse, parameters that characterize each of these separate factors usually cannot simply be “multiplied together” to understand their composed effects. They have to be filtered through dynamical models that properly account for depletion and saturation effects in populations. So it is understandable that the average person might have a hard time making sense of CDC estimates of such parameters, and it is not surprising that there are a lot of misconceptions and misperceptions about these topics.
Let’s take the CDC COVID-19 Pandemic Planning Scenario report (as of May 20, 2020). This looks like a simple document at first, but it may be difficult to understand how to pull all of these numbers together. For a variety of reasons, parameters of interest to epidemiologists are difficult to estimate from data. One method to mitigate issues with incomplete or noisy data is to make assumptions that help fill in the gaps, but then your analysis is only as good as your assumptions. To be conservative and to understand how sensitive predictions are to these assumptions, the CDC has come up with five different “scenarios” that stretch across a wide range of assumptions. To keep things simple, we will focus on “Scenario 5: Current Best Estimate”, which is the CDC’s best guess at where these epidemiological parameters are.
It is best to start with everyone’s favorite epidemiological parameter, R0. This is the so-called “basic reproduction number.” It is a measure of how fast a contagious infection can spread. R0 is the combination of three factors:
- The rate of interaction between an infectious (contagious) person and others in the population (referred to as “contact rate” below in some places)
- The probability that an infectious person will infect someone that they come in contact with
- How long an infectious person stays infectious (we assume that after this period, they are in a permanent recovered state where they are immune to further infection)
Essentially, R0 is a ratio of the rate that an infectious person infects others to the rate that an infectious person becomes well. This ratio can be interpreted as the number of people an infectious person infects before they themselves stop being infectious. If R0 is less than 1, then a disease will naturally die out because (on average) those infected will not be able to infect someone else before they become well. If R0 is greater than 1, then we have a so-called endemic. That means that the infectious disease will be constantly maintained at some background level; some fraction of the population will always be either currently infectious or recovered. Interestingly, this fraction is not 100%. As an infectious disease spreads through a population, the number of those who are susceptible to further infection declines to a point where it is rare for infectious individuals to encounter them (contacts with infected and recovered are far more common). This means that when susceptible individuals are rare, each infectious individual spreads less of the infection during the time window that they are infectious. This is the so-called herd immunity. A fraction of the population can stably remain susceptible because they are protected by the large numbers of others who have already had the disease and buffer them against contact with those who are currently infectious. The fraction of the population that will remain susceptible at the so-called endemic equilibrium is 1/R0. Likewise, the fraction of those in a population that must have been infected (or vaccinated, if possible) in order to achieve herd immunity is (1–1/R0). I should note that this simplified model assumes that infectious people eventually become recovered and stay that way; things get more complicated if immunity is not long lasting.
So what does the endemic equilibrium (“herd immunity”) look like for COVID-19 (assuming long-lasting immunity)? Here is what CDC estimates for R0.
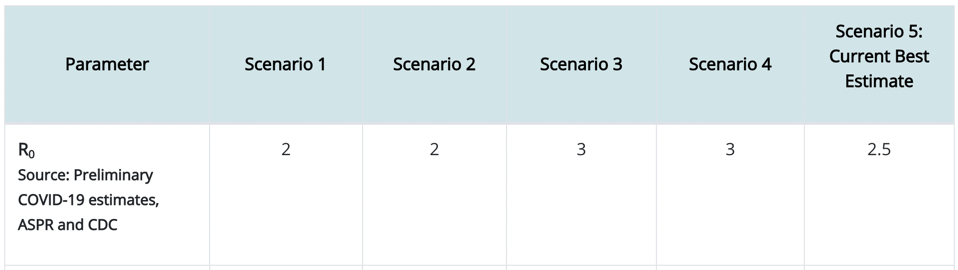
Again, focusing only on Scenario 5, we take R0=2.5, which means that any infectious person will have an opportunity to infect 2.5 other people on average. So we then estimate that 1/R0=1/2.5=40% of the population will be able to avoid infection so long as the other 60% of the population goes through an infection or is vaccinated. So exactly how many people is that? In the United States, the population is a little over 325 million people (compare this to the world population of 7.8 billion people). So that means that 60% of the 325M people in the USA must be infected to achieve herd immunity. That’s 195M people in the USA (4.68 billion people worldwide).
But not everyone who is infected sees symptoms let alone has to go to a hospital or suffers an early death. If we go back to the CDC data, we see that…
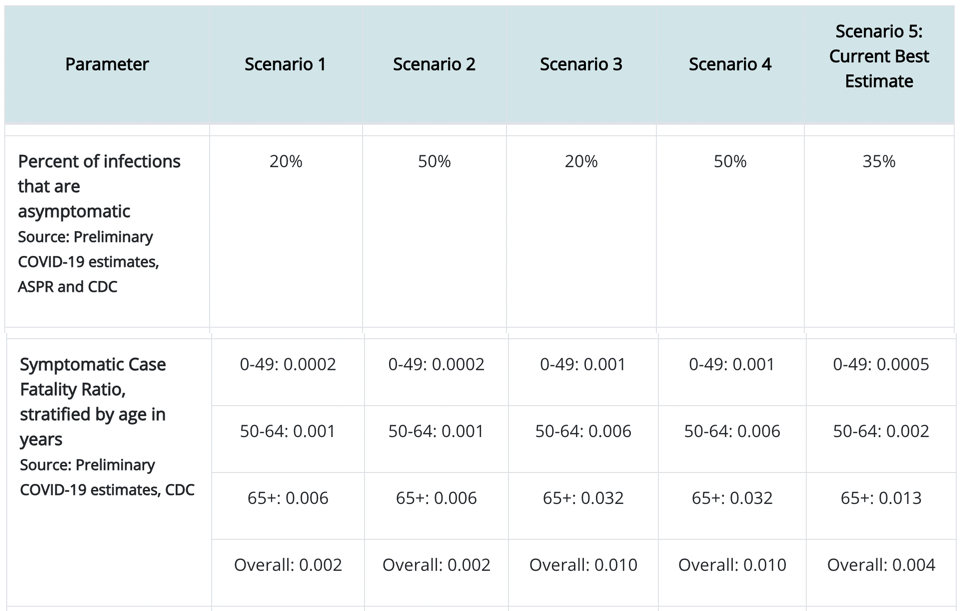
Again, looking at Scenario 5, we see that 35% of those who have an infection show no symptoms. We also see that those other 65% who show symptoms will suffer fatality at an overall (averaged across age groups) rate of 0.004 (i.e., 0.4%). That seems like a very small number! But we have to keep in mind that this is a very contagious disease (any infectious person infects 2.5 other people). So we need to combine the information on contagion with the information on case fatality rate. For the 325M people in the USA, we already calculated that 195M will have the disease. So then, at the endemic equilibrium (“herd immunity”):
- 195M*65% = 127M people will have shown symptoms in the USA
- 127M*0.4% = 508,000 people will die in the USA
And worldwide, we would expect 12.2M people will die. So even at that very small case fatality rate, there will be a lot of death (and even those that escape symptoms may still feel long-term effects of COVID-19 that we are only starting to understand now). Just as a reference, 38,000 people died in car accidents in 2018 in the USA. We try to prevent deaths by car accidents by preventing car accidents and trying to make cars safe so that people will survive accidents that happen. When we ask people to wear masks and social distance, this is not unlike people’s legal obligation to wear seatbelts and drive cars that meet safety standards.
Now, a lot of people say that there is no way to prevent these deaths, and so it is better to suffer them early instead of dragging out our march to the endemic equilibrium. In order to evaluate whether this is a good argument, we should take a look at another part of the CDC data:
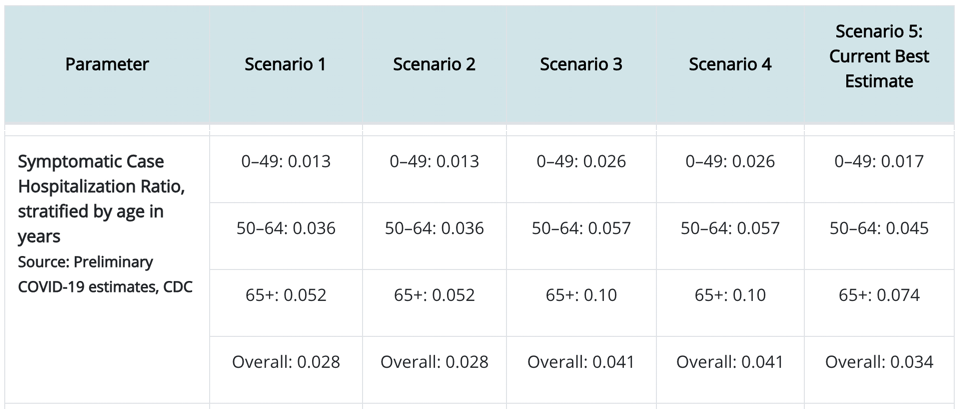
Focusing on Scenario 5’s “Overall” estimate, we see that each person who shows symptoms will have a 3.4% chance of being hospitalized. So that means we can estimate that for the population of 325M people in the USA, the 127M people we calculated above to show symptoms, 3.4% of them will have to be hospitalized, meaning that COVID-19 contribute 4.318M patients to hospitals in the USA (103M COVID-19 hospital patients worldwide). The question is whether we have enough hospital beds in the USA to accommodate these 4.318M people all at once. If we do not, then those that would have otherwise recovered will have to suffer through the disease without the support of medical professionals and medical technology. In other words, the case fatality rate for this subset of COVID-19 symptomatic individuals turned away from hospitals may rise to much higher than the 0.4% mentioned above. So this is really the essence of the movement to flatten the curve (e.g., by wearing masks and social distancing to reduce the effective contact rate). Even if it is impossible to avoid the 508,000 deaths predicted above, if infections can be spread out over a long amount of time, we can help to ensure that at any instant there will be enough hospital beds. Furthermore, if we stretch out the infection curve far enough, we may develop a vaccine within the curve’s duration. Vaccinations are a game changer because they provide a quick shortcut (that is hopefully much safer than a full-blown infection) to herd immunity.
But if we wanted to reduce that 508,000 without a vaccine, how would we do it? Remember that I said that R0 (a parameter of infection spread) is determined in part by the rate that an infectious individual contacts other individuals in the population. If we can devise long-term behavioral or technological methods to reduce this contact rate (beyond temporary inconveniences, such as wearing masks), then we can change R0 for COVID-19 for good (or at least for a sufficiently long time), thereby meaning that our endemic equilibrium (“herd immunity”) will occur with a much higher number of people who avoid infection (and even vaccination) entirely. How do we do that? Here are three potentially powerful ways.
- We can remove hand shaking and other similar kinds of contact as a greeting (thereby bringing the baseline contact rate for every individual in the population to a much lower level than it was before COVID-19).
- We can develop rapid, highly available, and frequent testing protocols that can quickly identify infected individuals so that they can be isolated (thereby bringing their personal contact rate much lower than others).
- We can develop sophisticated contact-tracing techniques that can further identify potentially infected individuals so that they can be isolated (thereby bringing their personal contact rate much lower than others).
These behavioral and technological changes can actually improve our long-term COVID-19 outcome even if a vaccine is not developed. So it may not be inevitable that hundreds of thousands of more people have to die (at the time of this writing, over 110,000 people in the USA had death certificates that indicated COVID-19 as a cause of death).
Medical professionals can develop vaccines, researchers can develop novel technologies, and we can all alter our behaviors. Unfortunately, there are additional challenges in the near future that will make all of this even more urgent. In particular, we are facing a flu season ahead of us. Individuals who contract COVID-19 and the seasonal flu simultaneously may be in an untenable situation. Additionally, the medical system will face demands not only from COVID-19 but from those with the flu (but possibly not COVID-19) who also need hospitalization. Normally the medical system would have enough capacity to serve the seasonal flu population (although there are still seasonal flu deaths every year, just not as much as COVID-19). However, if the medical system has to face flu and COVID-19 along with baseline demands and any other emergent demands (other pandemics, etc.), then that will put our society as a whole in an untenable situation. The flu shot may be especially important to encourage this season.
Of course, there are many other interesting figures in that CDC report that we could further analyze that relate to how long the average COVID-19 hospital patient takes to recover, which would help us figure out more quantitative details about the amount of each of the kinds of possible actions discussed above will be necessary to prevent hospitals reaching capacity. For now, I will leave that analysis as an exercise for the reader. In the meanwhile, get some rest, stay safe, and stay healthy!

